COVID Vaccines Still Save Lives. Here’s Why Hospitalization Protection Looks Lower.
The science behind changing effectiveness and why death protection remains strong.
A Turning Point That Didn’t End the Pandemic
When COVID-19 vaccines arrived in late 2020, they changed the course of the pandemic. Vaccinated people were much less likely to get very sick or die. Still, the pandemic didn’t end. Today, vaccines protect less against hospitalization than they once did. That shift can sound worrying, but it doesn’t mean vaccines failed. It means the virus and our immunity have changed over time.
What a New Study Shows
A large U.S. study published in JAMA Network Open in February 2026 helps explain what is happening now. Researchers studied nearly 8,500 adults hospitalized across 20 states during the 2024-2025 COVID season. They found that updated vaccines lowered the risk of hospitalization by about 40%. More importantly, vaccines reduced the risk of the most serious outcomes, needing a breathing machine or dying, by nearly 80%. Even when vaccines do not prevent hospitalization, they still protect strongly against death.
How the Virus Has Changed
One major reason vaccine protection has dropped is that the virus keeps evolving. The first vaccines were made to match the original virus and early variants like Alpha and Delta. But the virus to mutate. Omicron, which appeared in late 2021, had many mutations that made infections more common, even in vaccinated people. Newer variants like XBB, JN.1, KP.2, and LP.8.1 have continued this trend, making it harder for vaccines to block infection.
Why Immunity Fades
Vaccine protection also fades with time. After a shot, antibody levels rise quickly, then slowly fall over months. The immune system still remembers the virus, but it reacts more slowly. Many people counted as vaccinated in studies received their last dose six months or more earlier. Booster use has also dropped. This makes it easier for infections to become serious, especially during large waves.
What Hospitalization Means Today
Hospitalization does not mean the same thing now as it did early in the pandemic. In 2020 and 2021, many patients were admitted with severe lung damage. Later waves still led to many hospitalizations, but vaccines and prior infections changed who ended up in the hospital. Today, hospitalized patients are more likely to be older or have serious health problems. These groups often have weaker immune responses, which makes vaccines appear less effective against hospitalization. Many are admitted for monitoring rather than life-threatening illness. Hospitals also send patients home sooner, which affects how vaccine protection is measured.
The Big Picture
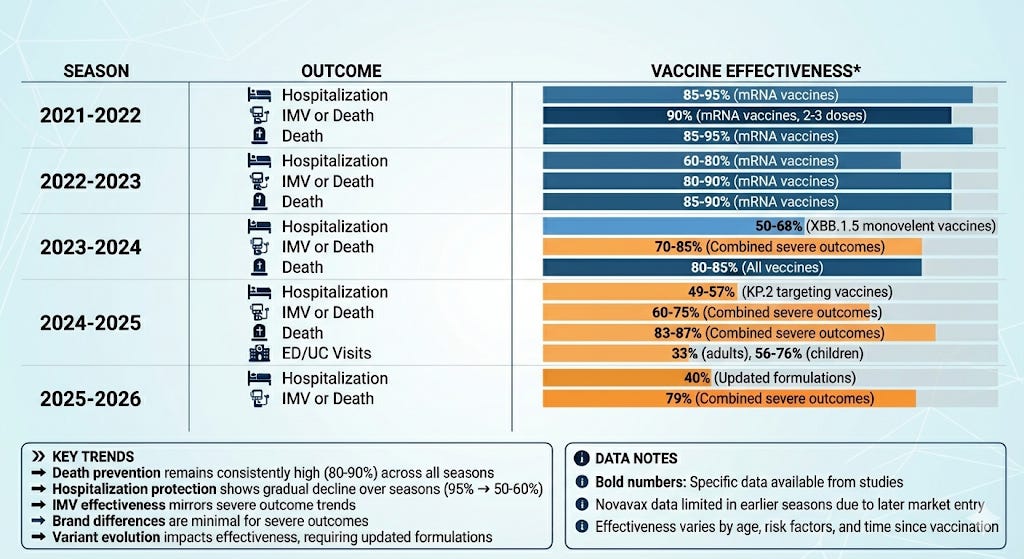
Over time, a clear pattern has emerged. In 2021 and early 2022, vaccines prevented about 85-95% of COVID hospitalizations. In later seasons, protection against hospitalization fell to around 50%. Protection against death, however, has stayed much higher, often above 80%. This is because deeper immune defenses, such as T-cell responses, remain strong and harder for the virus to evade.
These changes were expected. COVID vaccines are beginning to work more like flu vaccines. They won’t block all infections, but they greatly reduce the risk of dying. Cutting hospitalizations in half and preventing most deaths saves many lives. For now, vaccines remain our strongest tool for preventing the worst outcomes of COVID.
Table: COVID Vaccine Effectiveness (VE) Across Seasons
*VE for Pfizer, Moderna, and Novavax Vaccines
Sources:
Pfizer Reaffirms Safety and Efficacy of COVID-19 Vaccines, September 16, 2025.
Novavax’s Nuvaxovid 2025-2026 Formula COVID-19 Vaccine Approved in the U.S., August 27, 2025.
Important Limitations:
Some estimated ranges are based on trends from available surveillance data rather than specific published effectiveness studies.
2022-2023 season has fewer published formal effectiveness studies, so estimates are derived from ongoing surveillance systems.
Brand-specific data is limited in earlier seasons as most studies reported combined mRNA vaccine effectiveness.
Study methodologies vary across different surveillance networks and time periods.
Real-world effectiveness can vary significantly based on population characteristics, circulating variants, and time since vaccination.