Nearly Half of U.S. Adults Have Hypertension, and Most Aren’t Under Control
A new JAMA analysis shows that nearly four in five U.S. adults with high blood pressure remain above today’s treatment goal, revealing deep cracks in diagnosis, treatment, and follow-through.
America’s Hypertension Blind Spot
For many years, high blood pressure has been treated as something routine. It is checked at doctor visits, written down, and often forgotten. But a new study published in JAMA shows that this laissez-faire approach has come at a cost. Under today’s stricter guidelines, nearly 4 out of 5 U.S. adults with high blood pressure have numbers above recommended targets.
High Blood Pressure Is Widespread
The study looks at national health survey data from 2021 to 2023, at a time when heart disease is still the leading cause of death in the United States. Using the most up-to-date target of keeping blood pressure below 130/80, the researchers show how far the country is from turning medical knowledge into everyday care.
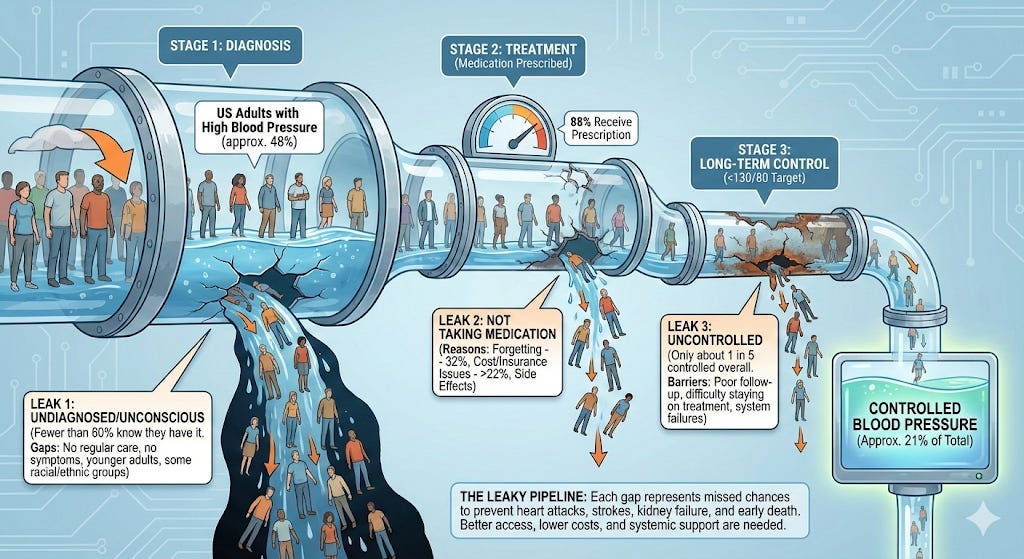
About 48% of U.S. adults now have high blood pressure. Yet only 59% know they have it. Just over half are being treated, and only 21% have their blood pressure under control. When the new goal is applied, 79% of adults with high blood pressure are above the target.
This does not mean high blood pressure has suddenly become more common. For years, using the older goal of 140/90, rates hovered at 28-30%.
The new guidelines lowered the target because strong evidence shows that lower blood pressure reduces the risk of heart attacks, strokes, and kidney disease. But the study makes one thing clear: changing the rules does not improve health on its own. Health systems, habits, and support need to change, too.
Care Often Stops with Diagnosis
Most people are diagnosed with high blood pressure during routine doctor visits. Those who see a primary care doctor regularly are far more likely to know they have it and get treated. Those without consistent access to care are often missed.
That gap shows up in the numbers. Fewer than 60% of people with high blood pressure know they have it. Because hypertension rarely causes symptoms, it can go undetected for years without regular checkups.
Uninsured adults and people who see doctors less often are more likely to have uncontrolled blood pressure. Younger adults, men, and some racial and ethnic groups are diagnosed less often, even as their long-term health risks quietly grow.
Medication: Prescribed But Not Always Taken
Among people who know they have high blood pressure, most are prescribed medication. Nearly 88% receive a prescription. On the surface, that sounds like success. But it hides another problem: many people do not take their medicine as prescribed.
The most common reason is forgetting. About 32% say they miss doses. Cost is another major issue. More than 22% struggle to afford their medication, and a similar share lack insurance. Side effects also play a role, even though many can be managed with different drugs or doses.
Here’s the key finding: among people who take their medication, about 72% reach healthy blood pressure levels. But because so many people are never diagnosed or stop treatment, only about 1 in 5 adults with high blood pressure is controlled overall.
A Leaky Pipeline
From a public health perspective, the diagnosis and treatment of blood pressure looks like a leaky pipeline. People drop out at every step, from screening to long-term control. Each gap means missed chances to prevent heart attacks, strokes, kidney failure, and early death.
Most adults with uncontrolled blood pressure are not taking medication at all. This does not mean doctors are failing. It often reflects a lack of insurance, high costs, poor follow-up, or difficulty staying on treatment over time.
These problems will not be fixed by guidelines alone. They require better access to primary care, lower drug costs, and systems that help people stay on track, such as simpler prescriptions, reminders, and community blood pressure checks.